Natural Remedies for Schizophrenia: Symptoms, Root Causes & Holistic Treatments
When exploring schizophrenia treatment options, many people discover that medication alone does not address the full complexity of the condition.

A Personal Note from George
Schizophrenia is, in my view, one of the most confronting and misunderstood mental health conditions a person can face. It doesn’t just affect the individual diagnosed — it can disrupt families, relationships, identity, and a person’s basic sense of safety in the world.
But here’s what many people don’t realise…
👉 Schizophrenia is not only about voices or hallucinations.
For many, the deepest suffering happens beneath the surface — a relentless internal struggle marked by fear, confusion, and often a profound depression that few people see.
For some, it feels like a war zone inside the mind — where inner conflict makes even simple daily functioning feel impossible.
Even with medication, many people feel emotionally numb or sedated, sleeping much of the day and struggling to reclaim motivation, clarity, or meaning. Adherence can become difficult — not because of resistance or denial — but because schizophrenia itself can interfere with insight, trust, and the ability to feel safe.
One of the most heartbreaking patterns I see is how often schizophrenia goes unrecognised in its early stages. Early signs are frequently mistaken for stress, trauma, substance use, or burnout. Only when symptoms intensify does the bigger picture become clear.
And this matters — because schizophrenia exists on a spectrum.
Some people experience milder functional impairment. Others face persistent hallucinations, paranoia, or long-term disability. Wherever someone falls on that spectrum, there is hope. With the right integrative and holistic treatment approach, stability can improve, distress can reduce, and quality of life can meaningfully change.
What Is Schizophrenia? A Functional View of the Condition
So, what schizophrenia is — and what it isn’t — is often misunderstood.
Schizophrenia is a complex psychiatric condition that affects how a person thinks, feels, and experiences reality. It may involve hallucinations, delusions, disorganised thinking, emotional blunting, or social withdrawal.
For many people searching for answers online, “schizophrenia is what?” is often the first question — asked during moments of confusion, fear, or uncertainty.
But here’s the key point:
👉 Schizophrenia is not just a label — and schizophrenia is not caused by one single factor.
From a functional perspective, schizophrenia is best understood as a multi-layered condition, shaped by overlapping biological, neurological, nutritional, genetic, psychological, and environmental influences.
This shifts the focus from simply suppressing symptoms to asking deeper questions:
- Why do symptoms emerge when they do?
- Why do they fluctuate?
- Why do some treatments help some people but not others?
While no single supplement can treat schizophrenia on its own, many people experience meaningful improvements when natural therapies are used alongside appropriate psychiatric care.
But here’s where things get interesting…
For some clients, targeted nutrient therapy helps reduce symptom intensity, improve stability, and soften medication side effects — especially when underlying biochemical imbalances are part of the picture.
This isn’t guesswork.
- Nutrient imbalances
- Neurochemical pathway disruptions
- Oxidative stress
- Chronic inflammation
- Trauma history
- Stress-response and nervous-system patterns
The goal isn’t to oversimplify — it’s to understand why schizophrenia presents the way it does for each individual, and to support stability, clarity, and wellbeing using a holistic, science-informed approach.

Signs and Symptoms of Schizophrenia

For many people, the early signs of schizophrenia are subtle and confusing — and for those living with schizophrenia, symptoms often don’t appear all at once, but emerge gradually, affecting daily functioning, relationships, and sense of self.
Symptoms usually become recognisable when they persist, intensify, or begin interfering with daily life.
Common symptoms may include:
- Hearing voices or sensory experiences others do not perceive
- Unusual beliefs or paranoia, such as feeling watched, followed, or unsafe
- Disorganised thinking or speech, where thoughts feel jumbled or difficult to express
- Flat or blunted emotions, with reduced facial expression or vocal tone
- Loss of motivation or difficulty completing everyday tasks
- Social withdrawal from friends, family, or work
- Loss of pleasure in activities that once felt meaningful
- Changes in sleep, appetite, or personal hygiene
Here’s the important part…
Symptoms don’t look the same for everyone.
- For some, they develop gradually.
- For others, they appear suddenly after a triggering event.
Symptoms may also overlap with:
- Trauma responses
- Bipolar disorder
- Substance use
- Extreme or prolonged stress
- Neurochemical imbalances
This is why a compassionate, functional assessment — one that looks beyond labels and explores biochemistry, nutrient status, neurochemistry, trauma history, and environmental stress — is often essential for understanding what’s really happening beneath the surface.
“I thought it was just stress…”
“I didn’t realise voices and mistrust could mean something deeper…”
“I’d seen five therapists before anyone suggested testing…”
Some people come across terms like “schizo schizophrenia” online — language that often reflects stigma or misunderstanding rather than the lived reality of the condition.
Natural Remedies for Schizophrenia: Are They Safe or Effective?

While no herb or supplement can treat schizophrenia on its own, many people experience meaningful improvements when natural treatments are used alongside psychiatric care.
But here’s where things get interesting…
For some clients, targeted nutrient therapy helps reduce symptoms, improve stability, or soften medication side effects — especially when neurochemical imbalances are part of the picture.
And it’s not just anecdotal.
“In peer-reviewed journals, psychiatrists are now acknowledging nutrient deficiencies in schizophrenia—particularly zinc, B6, and methylation cofactors—as factors that influence treatment success.”
Commonly Used Evidence-Supported Supports
When testing and clinical presentation suggest benefit, functional approaches may include:
- Zinc & B6 (P5P) — often helpful in undermethylation or pyroluria; supports neurotransmitter balance and oxidative stress reduction
- NAC — supports glutathione production and may reduce oxidative and inflammatory stress
- SAMe / methyl donors — used cautiously and only when indicated, based on methylation testing
- Magnesium L-threonate — supports neural calm and cognitive function
- Omega-3 fatty acids — support neuronal membrane stability and anti-inflammatory pathways
Important safety note: These therapies must be personalised. Certain supplements — particularly methyl donors — can worsen symptoms in some individuals if used incorrectly. This is why self-prescribing is not recommended, and functional testing plus professional guidance are essential.
Can You Recover Without Medication?
This is one of the most common — and most sensitive — questions.
The honest answer: complete recovery without medication is uncommon, and attempting to stop medication abruptly can be unsafe.
However, there’s more nuance than most people are told.
Many clients experience better clarity, fewer relapses, and improved daily functioning when medication is combined with targeted nutritional, biochemical, and stress-regulation support.
At BalanSoul, we don’t push people to stop medication.
We work with what’s already in place.
When clinically appropriate and medically supervised, gradual dose reduction may be explored — but always prioritising safety and stability.
For many people, the most effective approach is:
- Low-dose medication
plus - Targeted nutrient and functional therapy
Why this combination works:
- The brain stabilises more predictably
- Side effects are often reduced
- Long-term resilience improves
- Some clients maintain stability on lower doses over time
Every case is unique.
Every plan prioritises safety.

“What If It’s Not Schizophrenia?”
Here’s something rarely discussed:
Not all psychotic-like symptoms are schizophrenia.
Trauma responses, bipolar disorder, sleep deprivation, severe anxiety, B12 deficiency, heavy-metal exposure, histamine intolerance, and medication reactions can all mimic or overlap with psychotic symptoms.
That’s why, at BalanSoul, we consider all plausible causes — biochemical, neurological, nutritional, and environmental — before drawing conclusions.
Understanding why symptoms are happening is often the first step toward meaningful recovery.
Root Causes & Functional Medicine Approach to Schizophrenia
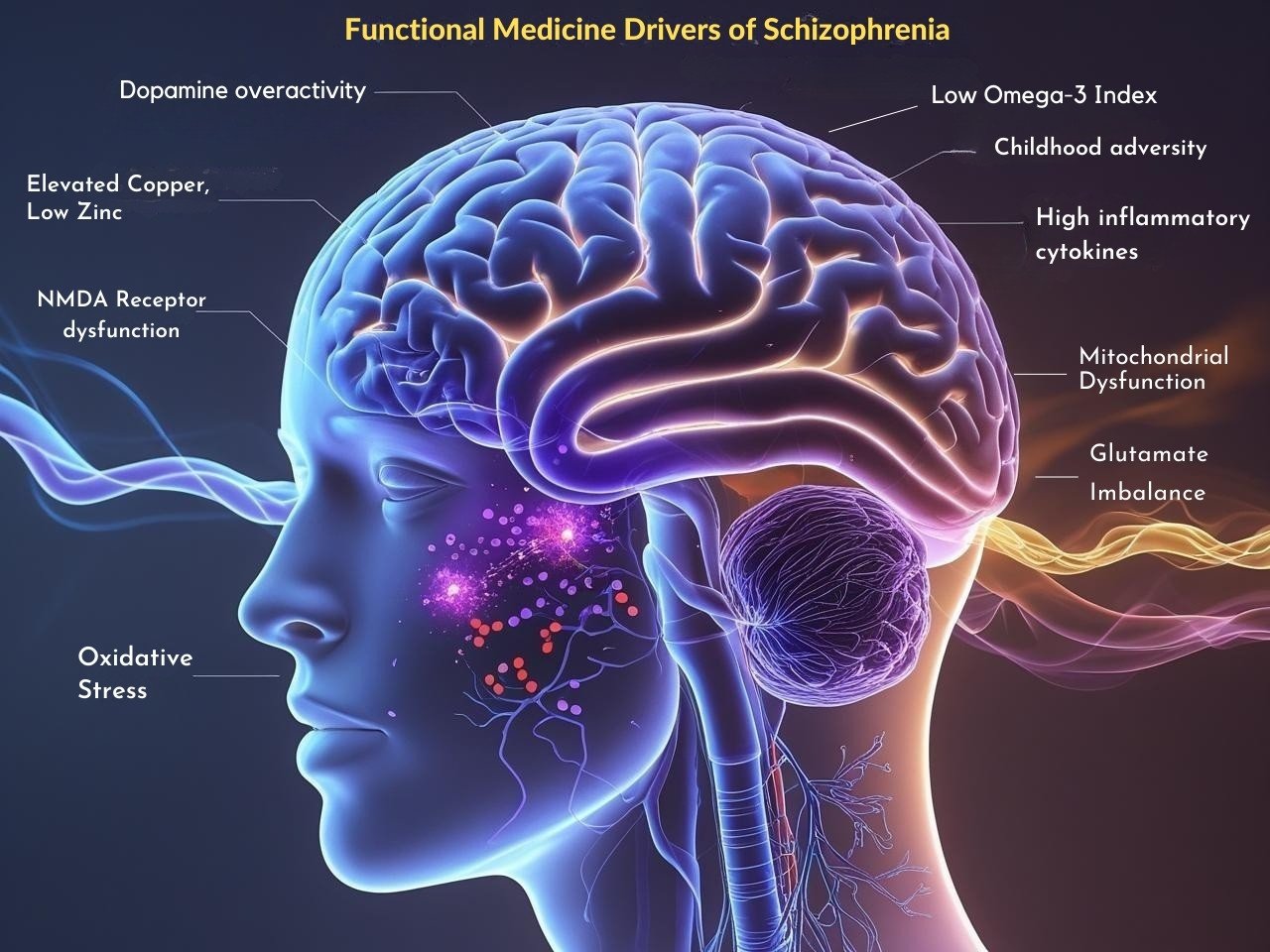
Functional medicine asks a different question.
Rather than focusing only on diagnosis, we ask a deeper and more personal question: what causes schizophrenia in this individual, at this point in time?
Not just:
“What is the diagnosis?”
But:
“Why is this happening in this person?”
Schizophrenia symptoms rarely appear in isolation.
In most cases, they emerge after the system has been pushed beyond its capacity — by a combination of biological vulnerability and life stressors.
At BalanSoul, we look beneath the label to understand the full web of contributing factors, which may include:
- Neurochemical and receptor imbalances
- Nutrient deficiencies affecting brain signalling
- Oxidative stress and mitochondrial strain
- Inflammation and immune activation
- Trauma or chronic stress exposure
- Genetic and epigenetic influences
Here’s the key insight:
Whether the dominant driver is copper overload, childhood trauma, oxidative stress, glutamate imbalance, or an undiagnosed pyrrole disorder — there is always a reason symptoms take the form they do.
And when those drivers are identified and addressed, the nervous system can stabilise.
This is why functional medicine moves beyond symptom suppression alone.
It allows us to design support that restores balance at the biochemical level — while also respecting the emotional and environmental context of the person’s life.
That deeper understanding is what makes targeted testing, biotype identification, and personalised treatment possible.
Key Root Contributors to Consider:
1. Neurochemical & Receptor Imbalances
- Dopamine overactivity — often linked to hallucinations, paranoia, psychosis, and intrusive thought
- NMDA receptor dysfunction — contributes to cognitive decline, thought disorganization, and dissociation
- Glutamate imbalance — elevated levels may trigger excitotoxicity, agitation, and panic-like states
2. Nutrient & Genetic Factors
- Elevated copper / low zinc — disrupts neurotransmitter balance, increases oxidative stress
- B6, B12, and folate deficiencies — impair methylation, myelination, and neurotransmitter synthesis
- Methylation imbalances (under- or overmethylation) — alter serotonin, dopamine, and histamine pathways
- Folate intolerance / methylfolate sensitivity — may worsen symptoms in sensitive biotypes
- Pyrrole disorder (Pyroluria) — leads to chronic B6 + zinc loss, emotional dysregulation, irritability, and dreamlessness
- Impaired SAMe / SAH ratio — signals blocked methylation cycles often seen in complex psychiatric cases
3. Inflammation, Oxidative Stress & Cellular Energy Deficits
But what happens when the brain becomes overwhelmed by inflammation and oxidative pressure?
These pathways begin to break down.
- High inflammatory cytokines — linked to cognitive fog, mood instability, and fatigue
- Elevated quinolinic acid — neurotoxic metabolite associated with suicidality and NMDA overactivation
- Mitochondrial dysfunction — reduces neuronal energy output and stress tolerance
- Low Omega-3 Index (EPA/DHA) — affects membrane fluidity, neurotransmitter signalling, and neuroprotection
4. Gut–Brain Axis Disruption
And here’s something many people overlook:
The gut profoundly influences neurotransmitter function.
- Dysbiosis & intestinal permeability — can trigger systemic inflammation and serotonin disruption
- Antibiotic use in childhood or repeated courses — may alter microbiome diversity and future stress resilience
5. Environmental & Trauma-Linked Contributors
Consider this:
The brain is shaped by the environments it is exposed to — especially early in life.
- Childhood adversity, neglect, or attachment rupture — sensitizes the limbic system and stress circuits
- Mould, chronic infections, or toxic exposures — can provoke neuroinflammation in susceptible individuals
- Heavy metal exposure (lead, mercury, arsenic) — associated with cognitive decline and psychosis-like symptoms
6. Structural & Metabolic Disruption
- White matter loss & myelin sheath damage — seen in long-term schizophrenia; linked to B12 deficiency and oxidative stress
- Elevated homocysteine — signals methylation impairment and correlates with cognitive dysfunction
⭐ The Bigger Picture
Schizophrenia is not a “single-pathway” condition — it is a mosaic of biochemical, genetic, neurological, environmental, and emotional factors.
And this leads to a crucial insight:
No one treatment can fully resolve it.
The most meaningful improvements occur when we address healing from every angle:
- restoring nutrient balance
- calming neuroinflammation
- supporting neurotransmitter pathways
- repairing gut integrity
- strengthening stress regulation
- integrating mind–body therapies
- and addressing social and emotional layers of the person’s story
This is where functional psychiatry shines. At BalanSoul, we specialise in connecting the dots — uncovering what standard approaches may overlook, not just managing symptoms but understanding why they appeared. When we treat the person, not just the diagnosis, real recovery becomes possible.
The Walsh Protocol & Functional Testing for Schizophrenia

“Schizophrenia isn’t one disease — and it can’t be solved with one drug.”
– Dr. William J. Walsh, PhD
At BalanSoul, we look beyond diagnostic labels to uncover the biochemical drivers of schizophrenia.
But why does this matter?
Because many individuals with schizophrenia-spectrum symptoms show distinct, measurable patterns in their brain chemistry — patterns that standard psychiatric assessments rarely detect.
The Walsh Protocol — based on over 30,000 cases — shows that many individuals with schizophrenia-spectrum symptoms present with distinct, measurable patterns in brain chemistry.
According to Dr. Walsh’s clinical database, more than 60% of individuals with schizophrenia exhibit significant methylation imbalances or related nutrient-pattern abnormalities often missed in standard care.
And here’s the key insight: These patterns aren’t theoretical. They influence how someone responds to medications, folate, SAMe, B6, or even environmental stress — and often explain why conventional treatment alone doesn’t always stabilize symptoms.
Let’s explore the most common biotypes seen in schizophrenia.
Common Biotype Patterns in Schizophrenia (Walsh Model)
Overmethylation + Excess Dopamine
- Seen in paranoid schizophrenia and delusional states
- Traits: high dopamine, low histamine, religiosity, sensory amplification, panic, grandiosity
- 🧠 Support: Folate, B12, niacinamide, DMAE, zinc
- ⚠️ Caution: May worsen with SAMe or methyl donors
Copper Overload
- Elevates norepinephrine → fuels paranoia, inner agitation
- Common in females, especially postpartum or on birth control
- 🧠 Support: Zinc, B6, selenium, MT-promoting nutrients
- ⚠️ Must decopper slowly to avoid irritability spikes
Pyrrole Disorder
- Depletes zinc and B6 → leads to dreamlessness, inner tension, emotional fragility
- 🧠 Support: High-dose P5P, zinc, biotin, GLA
- 📈 Often rapid improvement with targeted protocol
Undermethylation (in some subtypes)
- High histamine, low serotonin → may present with OCD traits or emotional flatness
- 🧠 Support: SAMe, methionine, zinc, magnesium
- ⚠️ Avoid folate unless carefully supervised
Recommended Testing

We test — not guess.
But what does this mean for you?
It means your treatment plan is guided by data, not assumptions.
Using advanced functional lab analysis, we identify your biotype and build targeted nutrient plans based on your unique biochemical fingerprint.
Typical Walsh-related tests include:
- Zinc : Copper Ratio (plasma) — copper retention pattern
- Ceruloplasmin — detects hidden copper loading
- Whole Blood Histamine — methylation status
- Pyrrole Test (HPL urine) — oxidative stress & B6/Zn demand
- SAMe : SAH ratio, B6, MTHFR / COMT SNPs — methylation capacity
- OAT Test — neurotransmitters, inflammation, oxidative stress
Why This Testing Matters
Medication can reduce symptoms — but without biochemical support, progress often plateaus.
Many clients are told they’re “treatment-resistant,” when in reality their brain chemistry hasn’t been properly matched.
Once a biotype is identified, we can:
- Support medication response rather than working against it
- Reduce side-effect burden
- Improve stability, resilience, and long-term outcomes
Functional testing gives us clarity — not just about what is happening, but why.
And when we understand the “why,” meaningful progress becomes possible.
Why Choose BalanSoul — And What to Expect When Working With Us
Schizophrenia doesn’t just affect perception — it can disrupt identity, trust, motivation, relationships, and a person’s sense of safety in the world.
That’s why our care is personal, measured, and deeply human.
At BalanSoul, we don’t rush decisions or apply one-size-fits-all protocols. We walk with you patiently, strategically, and compassionately — whether you’re newly diagnosed, medication-sensitive, supporting a loved one, or searching for a deeper, integrative approach.
Your Initial Consultation (90 Minutes)
Your first session is a comprehensive 90-minute consultation — not a quick check-in or surface-level discussion.
This time allows us to truly understand the whole picture, including:
- Mental health history and symptom timeline
- Medication use, responses, and sensitivities
- Periods of stability, relapse, or functional decline
- Nutritional status, stress load, sleep, and nervous-system patterns
- Relevant lab results or previous testing
- Your goals, concerns, and pace preferences
This depth gives us clarity — so we move forward safely, thoughtfully, and proactively, rather than reactively.
What You’ll Receive
Based on your history, biochemistry, and current stage, you’ll receive:
A personalised care plan, grounded in functional and biochemical assessment
Targeted nutrition and supplement guidance, aligned with Walsh Protocol and functional psychiatry principles
Clear education, so you understand what’s happening — and why
Nervous-system and lifestyle support tailored to stability, rhythm, and resilience
A step-by-step roadmap, not a generic protocol
Our focus is always on addressing root causes, not just suppressing symptoms.
Ongoing Support (Not One-Off Care)
Schizophrenia — and recovery — is rarely linear. Neither is our care.
As you move through each phase, we continue to:
Adjust nutrients and strategies as your system responds
Support nervous-system regulation and emotional stability
Help distinguish temporary setbacks from true relapse
Refine your plan using real-time feedback, not assumptions
This is collaborative care, at your pace — focused on restoring trust in your body, not forcing change.
There is a path forward — one step at a time.
With informed, compassionate support, stability can improve, cravings can soften, and clarity can return.
You don’t have to rush.
You don’t have to push.
And you don’t have to do this alone.
Click below to explore our testing options or book a free discovery call.
FAQ
Can I still take medication?
Yes. We support both medicated and unmedicated clients. We work with your existing care team to ensure safety and integration.
What if I’ve been misdiagnosed?
We assess your symptoms through a functional medicine lens. Not every case of paranoia or hallucinations is schizophrenia — and sometimes testing reveals underlying drivers like B12 deficiency or trauma-related dissociation.
Is this safe for my adult child or elderly parent?
Yes — all plans are tailored to the life stage and functional ability of the client.